History offers little guide to how we should escape from Covid’s clutches
When at the beginning of the coronavirus pandemic China placed a cordon sanitaire around Wuhan and then quickly extended it to eight other Chinese cities, placing 45 million people under lockdown, the immediate response was that it could never happen here. Even though quarantines have been employed in Europe since the 14th century, few of us thought the citizens of mature western democracies could be persuaded to accept similar restrictions. It seemed like a measure from the dark ages.
That imaginative failure arguably lay at the heart of Britain’s decision to pursue a herd immunity strategy during the early weeks of the pandemic by letting the virus run through the population, rather than locking society down tightly in an effort to suppress infections and prevent hospitals being swamped.
Today, we know better. In the absence of vaccines, quarantines were our only realistic option. Sure, there have been fines here and there for breaches of stay-at-home orders and occasional protests, but by and large Britons have acceded to the measures with remarkable grace.
But now, or at least from 19 July, we are supposed to make our own judgments as to when to mask up and when to self-isolate. The exhortation to “learn to live with Covid” casts each one of us as part moral philosopher, part health economist, making finely tuned decisions about what is an acceptable risk and our responsibility to our fellow citizens. As anyone who has wrestled with the decision whether or not to deactivate the NHS Covid app can attest, it’s an ethical minefield.
In Australia, however, where just 6% of the population has been double-jabbed, it’s a different story. There, residents of Sydney, Perth and Brisbane are enduring another gruelling round of stay-at-home orders in an effort to suppress surging infections sparked by the Delta variant. Meanwhile, in New Zealand – so long the poster child for the elimination approach to Covid but where only 10% of the population has been vaccinated –hospitals are seeing an influx of babies with a potentially deadly respiratory virus. No one is sure what lies behind the sudden rise in cases of respiratory syncytial virus, or RSV, but it seems likely they are the product of a phenomenon known as “immunity debt” – where people don’t develop immunity to other viruses suppressed by Covid lockdowns, causing cases to explode months later.
It is a sobering reminder of how the coronavirus, and access to vaccines, has divided our world and how quarantines are not without their own health consequences. Little wonder that now 60% of Brits have been double-jabbed, Boris Johnson has had enough of these finely tuned decisions and is seeking to pass the buck to you and me.
But can it be so easy to call time on a pandemic that is the cause of four million deaths and rising?
There has only ever been one way of exiting this pandemic and that is through herd immunity. The question is how to achieve this as quickly as possible without sinking the economy and while keeping the loss of life to a minimum.
Should we rely on vaccines to do this job or continue to employ a mix of measures and, if so, can citizens be trusted to become arbiters of which measures to adopt, when?
One hundred years ago these dilemmas did not arise. With the exception of smallpox, there were no vaccines against viral diseases and, although in 1918 scientists attempted to make a vaccine against Spanish flu, their efforts proved unsuccessful. Instead, prioritising the wartime economy, people were left to find their own accommodation with the virus as infections spread through the population.
Given the uneven global distribution of vaccines, the need for social distancing and quarantines has not gone away
Even when it became possible to manufacture vaccines against influenza, as was the case during the 1957 and 1968 pandemics, it was thought there was little possibility of developing vaccines against new strains in time. Calculating that at most one quarter of the population would be infected, the viruses were permitted to run their course.
Today, whether we realise it or not, descendants of the H1N1 Spanish flu and other pandemic viruses continue to circulate. Sure, every season they mutate a little and vaccines have to be updated, but while some people, mostly the elderly, continue to die, the rest of us have learned to live with the threats. The viruses are no longer epidemic but endemic.
This is the endgame most scientists envisage for Covid, hence the talk of “booster vaccines” and follow-on jabs to address mutations.
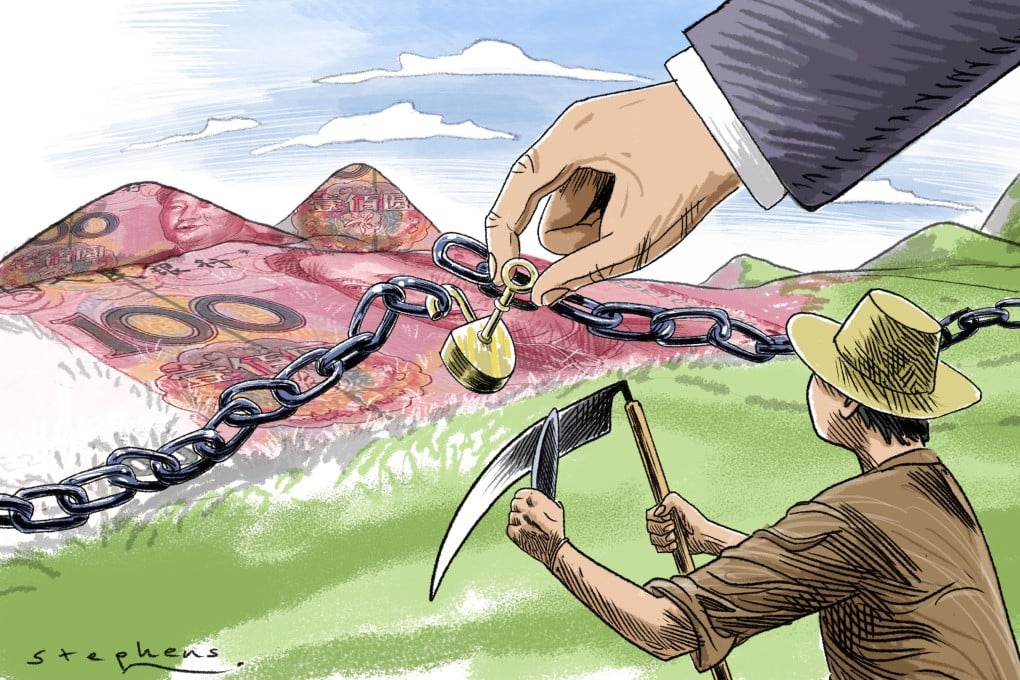
In the meantime, however, given the uneven global distribution of vaccines and supply bottlenecks, the need for social distancing and quarantines has not gone away. This is particularly the case in low- and middle-income countries in Africa, Asia and Latin America, where, despite the World Health Organization’s (WHO) Covax initiative, vaccine supplies fall far short of what is required to reach the Elysian fields of herd immunity. Instead, those countries are fertile breeding grounds for the Delta and other variants.
The problem is that as long as the virus continues to run wild anywhere, there is a risk of someone becoming infected with an emerging variant resistant to vaccines and unknowingly introducing it to another country, potentially undermining the effectiveness of that country’s vaccination programme. As Tedros Adhanom Ghebreyesus, the director of the WHO, puts it: “No one is safe, until we are all safe.”
The tragedy is that it has taken far too long for the world to wake up to this fundamental biological fact.
• Mark Honigsbaum is the author of The Pandemic Century: A History of Global Contagion from the Spanish Flu to Covid-19