‘We need to respect the process of healing’: a GP on the overlooked art of recovery
Over the past two years I’ve spent much of my time as a GP assessing and managing the fear, fever and breathlessness caused by coronavirus, but I’ve also spent more of my time than ever before talking to people about recovery and convalescence – not only from the virus, but from the damaging effects of repeated lockdowns. I’m a GP in central Edinburgh and, with three other doctors and two nurses, provide medical care to about 4,000 patients.
The words “recovery” and “convalescence” were rarely mentioned during my six years of medical school and seven years of specialty training. Many of my tutors seemed to assume that once a crisis of illness has passed, the body and mind find ways to heal themselves. But nearly 20 years as a GP has shown me time and again that the reverse is true: guidance and encouragement through the process of recovery can be indispensable.
‘We need to respect the process of healing’: a GP on the overlooked art of recovery – podcast Read more
My medical training took for granted a western medical approach to the body. But illness is not simply a matter of biology, but also one of belief, psychology and sociology. The ways we get ill are as much about culture as they are about disease, and our ideas and expectations of the body profoundly influence the ways in which we fall ill, and the ways we recover. I have learned much from those other clinicians – the nurses, physiotherapists and occupational therapists – who have most helped my patients, and I am constantly being reminded of how much more there is still to learn.
Get the Guardian’s award-winning long reads sent direct to you every Saturday morning
What follows, then, is a discussion of recovery and convalescence as seen from within a particular medical tradition – my own as a 21st-century European general practitioner. While I acknowledge the value and the virtues of alternative approaches to the body and to illness, I will leave discussion of them to others trained in their use.
It was on 31 December 2019 that the Chinese government alerted the World Health Organization to a new and dangerous strain of coronavirus that was infecting people in and around Wuhan. Humanity has learned an enormous amount over the subsequent two years – new ways of managing the pneumonia caused by the virus, as well as how to build a suite of vaccines proven to be effective against it. We move into this new year still struggling to contain a pandemic many thought would be over by now. New, more transmissible and more dangerous strains of coronavirus are still emerging. As they put our powers of recovery to the test, it’s worth thinking more deeply about what convalescence really means.
When I was eight years old, I woke one autumn morning with a hammer-blow headache and a churning in my stomach. My GP was called for – a kindly man of the old school who took one look and, suspecting meningitis, sent me urgently to an infectious diseases hospital an hour’s drive away where the diagnosis was confirmed. I spent eight days and nights in that hospital, in a room with large windows that gave on to trees and bright afternoon sunshine.
In the niches of my memory I carry no images of the doctors, only one of a nurse in a sky-blue tunic, her black hair in a bun, her kind face lined with smiles. I remember an iron-framed bedstead, glaring white sheets and the smell of floor disinfectant. A window in an internal wall of the sickroom looked on to a nurses’ station – I was kept under continual surveillance. Though my mum and dad took shifts to be with me for most of the day, they also had my brother to attend to, and I spent many hours alone in silence waiting for them to come; waiting for home.
A couple of years later, I broke my leg and was obliged to pass the whole of the summer holidays and part of the autumn school term in plaster. Beneath that plaster my leg withered and, when the plaster came off, I remember being shocked by how pallid, stunted and weakened it had become. Again, I don’t remember any of the doctors involved in my treatment. My recovery was led by a pair of brisk and cheerful physiotherapists.
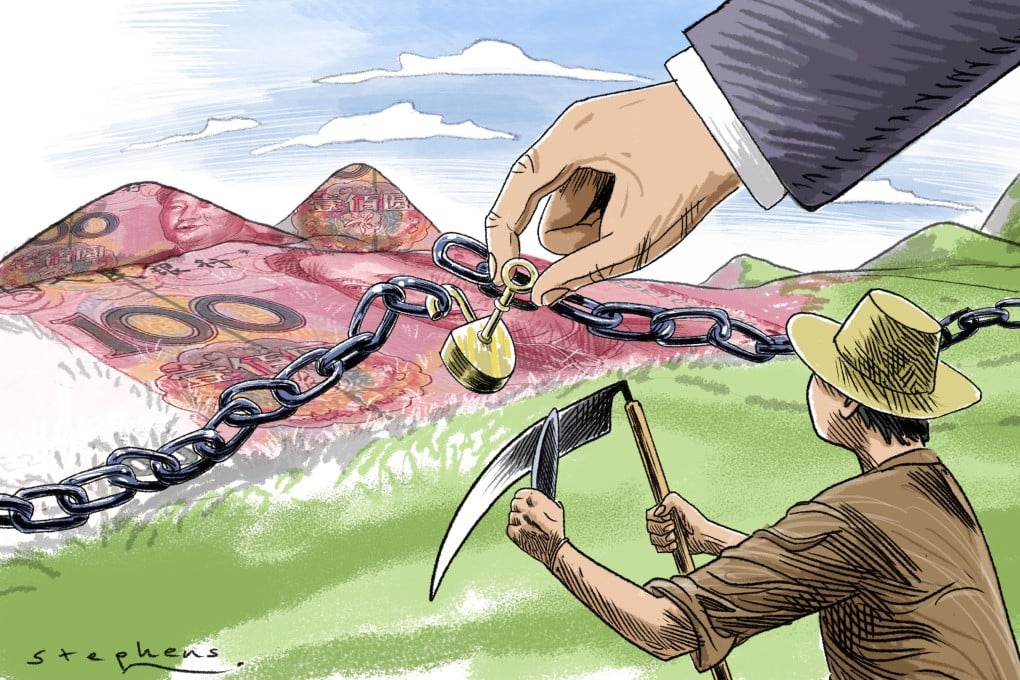
Facebook Twitter ‘With a limb, it seemed possible to objectify the part that needed recovery’ … Photograph: piola666/Getty Images/iStockphoto
With a limb, it seemed possible to objectify the part that needed recovery, to look down on the leg and say “that’s the problem, right there”. My progress was effortful, but at least I could see it, inscribed in the bulk of my thigh and the colour of my skin. My recovery from meningitis was far more difficult to grasp – the edges of what recovery meant were far less clear. A languorous, fuzzy-headed exhaustion dominated my days, burnishing the world with the bright haze of a dream or hallucination. My body was in convalescence, but the process itself felt disembodied, ethereal, as much mental as physical. As I look back on it now, it’s clear that it was my first experience of the complexities of convalescence, and how it can and must take very different forms with different illnesses and between different people.
The word “rehabilitation” comes from the Latin habilis, meaning, among other things, “apt” or “fit”, and carries the sense of restoration: “To stand, make or be firm again.” The aim of rehabilitation, then, should be to make someone as fit as they can be – to stand on their own feet if they’re able, and to recover as much mobility and independence as possible if they are not. I worked once as a junior doctor in a unit dedicated to rehabilitation from brain injury, and learned there that convalescence is anything but a passive process. Though its rhythms and its tempo are often slow and gentle, it’s an act, and actions need us to be present, to engage, to give of ourselves. Whether it’s our knees or skulls that need to heal from an injury, or lungs from a viral infection such as Covid-19, or brains from a concussion, or minds from a crisis of depression or anxiety, I often have to remind my patients that it’s worth giving adequate time, energy and respect to the process of healing.
There is no hierarchy to suffering, and it’s not possible to say of one group of conditions that they deserve sympathy while another group deserves to be dismissed. I’ve known patients whose lives have been dominated for years by the grief of a failed love affair, and others who have taken the most disabling injuries, pain, indignity and loss of independence in their stride. Though it can be tempting to resent someone whose illness appears to be less serious than our own, or to judge ourselves harshly when others seem to be coping with more challenging circumstances than we are, comparisons are rarely helpful. Neither is it advisable to set out a strict timetable of recovery: it’s more important to set achievable goals. Sometimes, all I can do is reassure my patients that I believe improvement of some kind is possible. The recovery I’m reassuring them of might not be biological in nature – in terms of a resolution of their condition – but rather an improvement in their circumstances.
In the course of my medical work I sometimes see viral infections sending their sufferers to bed for weeks or months, and, in a few cases, for years. Why this happens is poorly understood. It’s as if the struggle with illness draws so deeply on one’s inner reserves of strength that the body does all it can to retain its energies, even going so far as to manipulate our sense of effort so that to take a short walk, or to climb a flight of stairs, is to risk exhaustion. Through the successive waves of Covid-19 during 2020 and 2021, I spoke to many patients in whom coronavirus has triggered this kind of enduring fatigue. A letter in the journal Nature Medicine published last March reported that, for their sample group, one in eight victims of Covid-19 suffered symptoms lasting longer than four weeks, one in every 22 had symptoms lasting longer than eight weeks, and one in 44 patients had symptoms lasting longer than 12 weeks. The most persistent symptoms were breathlessness, loss of smell, headache and fatigue.
Physiotherapists encourage people experiencing relentless post-viral fatigue to gently push at the limits of what they can do in terms of physical effort. They’ve found that if those limits are not tested, then the realm of the possible begins to shrink – horizons contract, muscles weaken and sufferers can become trapped in a cycle of effort followed by collapse. The effort required to provoke each collapse begins to dwindle.
Everyone has a different tempo of convalescence, and will require different strategies. It’s normal that the process can be slow, and normal, too, for long-term illness to vary in its manifestations from person to person. Protracted symptoms from viral infections may differ enormously between different individuals, but can include varying amounts of breathlessness, difficulty concentrating, forgetfulness, mood changes, insomnia, weight loss, weight gain, exhaustion, muscle weakness, joint stiffness and flashbacks. When I see patients troubled by these kinds of problems, I try to emphasise that to experience them isn’t evidence that recovery has stalled, or is going into reverse. On the contrary, those symptoms are evidence that the body and mind are reacting and changing in response to the illness – and where there’s change, there’s hope. There is a booklet I hand out to people with ongoing symptoms of Covid-19, written by local physiotherapists, that emphasises the importance of this “pacing” approach to recovery. It’s an attitude I’ve benefited from myself.
Facebook Twitter Patients recovering from coronavirus perform breathing exercises with a physiotherapist. Photograph: Dimitar Dilkoff/AFP/Getty Images
During my first year in training as a GP, I got sick. I’d worked for many years in hospitals, had already qualified as a trainee in emergency medicine, but the intensity and breadth of problems I was learning to face in my new role as a doctor in the community felt to me almost overwhelming. An old problem with my sinuses flared up, leaving me with a ceaseless, drilling headache above the eyes that sapped all of my energy. I was exhausted, couldn’t concentrate and was in chronic pain. An MRI scan showed that I needed surgery, which might take months to arrange. In the meantime, I had my GP training to complete.
I couldn’t do anything to speed the arrival of my operation date, but I could do something about my exhaustion and my levels of stress. Rather than stop work altogether, I reduced my hours to a three-day week – each day in clinic would be followed by a day off to recover. The headache was as bad as ever, but with more time to rest and recuperate between clinic days, the pain bothered me less. Knowing I’d have the breathing space of a day at home meant that I was able to give my best to my patients on those days I was in the clinic. My training would be delayed – it would now take longer than a year for me to be signed off as a competent GP – but I persuaded myself that there was no point risking burnout for the sake of a schedule of someone else’s making.
And I qualified all the same, albeit a couple of months late. The operation, when it came, was successful, my headaches were cured, and I had learned a valuable lesson. We need strength and energy to live with illness. Cutting my workload gave me the reserves I needed not just to live with chronic pain until the operation, but to begin slowly on the path towards recovery from it.
All worthwhile acts of recovery have to work in concert with natural processes, not against them. Many antibiotics don’t “kill” bacteria as such, but merely inhibit the growth of bacterial colonies and leave the body to do the rest. A doctor who sets out to “heal” is in truth more like a gardener who sets out to “grow” – actually, nature does almost all the work. Even when I stitch a patient’s wound, the suture material itself does not knit the tissues – that thread is simply a trellis to guide the body in its own work of healing.
This idea of the body as belonging to the green, organic world is something often forgotten in the clinics and hospital wards where I’ve trained and worked – so much so that it came as a surprise to read of a physician who has taken it to the heart of her clinical management. Victoria Sweet is an associate professor of medicine at the University of California in San Francisco. For many years she worked in one of the last almshouses in the United States – a hospital for the poor who have nowhere else to go.
Sweet’s book God’s Hotel: A Doctor, a Hospital and a Pilgrimage to the Heart of Medicine explains how, after reading about the medieval healer Hildegard of Bingen, she came to the conclusion that, to better describe the aims of recovery, we should resurrect Hildegard’s medieval concept of viriditas, or “greening” – to be healed is to be reinvigorated by the same force that gives life to trees as much as it does human beings. She, too, observed that the work of the physician is much more like that of a gardener than it is like a mechanic.
This makes intuitive sense: until very recently, physicians had to study botany, not only because so many medicines are derived from plants, but because the study of plants is a way to understand life itself. The GP I had as a child – the one who sent me urgently to hospital with meningitis – told me later that he had to take botany classes as part of his medical school curriculum in the 1950s. It is as if, with the pharmaceutical revolutions of the later 20th century, we have forgotten something of the importance of a broader approach to recovery. It has been shown that patients recovering in a hospital bed need less pain-relieving medication if they have a view out over something green, growing and alive. This was recognised long ago by Florence Nightingale, but seemingly forgotten by the modern architects of our hospitals.
The word “physician” can be rooted back to the Greek physis, meaning “nature”, and phuo, which means “to grow”. Just like a plant, what we need in order to grow back into wholeness is a “regime” of the right nutrients, the right environment and the right attitude – and to be left in peace. This attitude to recovery has been crowded out in modern medicine because it takes time. Sweet wouldn’t want to return to medieval medicine, and wouldn’t give up our blood tests and scans, our robotic surgery or antibiotics. But she would like to see the value of time restored to the practice of medicine – and so would I.
Doctors and nurses bring their own personalities and experience to every medical encounter, and we know that people recover more quickly from physical conditions if they perceive their clinician to be sympathetic to their concerns. Psychological research into “compassion fatigue” has shown that most students begin clinical studies with a great deal of compassion, but the longer they work in caring professions, the more they seem to lose it.
The word “doctor” comes from docere, meaning “to teach” or “to guide”, and just as every teacher you’ve ever had works with a different style, so does every doctor. The idea that there’s a universal approach every practitioner should adopt is false, and would be a terrible way to offer medical care. In the 30 or 40 medical encounters I have in the course of a normal working day, there must be several that I misjudge, guessing wrongly which kind of doctor that particular patient needs me to be.
I’m not sure this kind of intuition is something that can necessarily be taught. But what can be taught is the confidence to act on the small voices of conscience and experience that suggest when a therapeutic relationship will benefit from going off-piste – away from the well-trimmed paths of textbook solutions into something wilder, more unscripted and perhaps more effective. Within modern medicine, this creates a conflict, between an idea of a clinical encounter that should be measurable, reproducible and thus open to professional regulation of standards, and the idea of the clinical encounter as an alchemy that combines the experience of two human beings in an unrepeatable moment that changes both of them.
Doctors have to be well grounded in the science of medicine – that isn’t up for debate. But what is open to question is whether scientific knowledge is where medical practice ends, or where it begins. The answer might of course be different in different situations. I have some patients who see me solely as the conduit through which to gain access to specialists, and others who want from me, as a representative of the medical establishment, the scientific facts of their particular condition. And at the other end of the spectrum I’ve known patients for whom the aim of our consultations is to feel cared for, and to be given a sense of confidence in their recovery even when their condition is one that can’t be cured. Just as some people need to understand the science of their disease in order to better appreciate how to defeat it, others need to understand illness as a story that is tending towards a happy ending. I’m happy to take whichever approach the patient prefers: the biology of an illness, or its biography. Both are equally valid ways of approaching medical encounters. Similarly we would do well, as a profession, to expand the notion of what counts as a therapy.
Facebook Twitter A Covid patient in Spain recovering with the help of two health workers. Photograph: Pierre-Philippe Marcou/AFP/Getty Images
Drugs can be the least of healing, and the idea that therapies must be something that you swallow or inject – that they should be pills or syrups or infusions – is manifestly untrue. I’ve seen choirs, walking groups, gardening clubs and voluntary work revolutionise the health of patients of mine, and there are many opportunities, frequently unexploited, for patients to become their own best physicians, often with the help of non-medical agencies.
Similarly, there can be non-medical solutions that help greatly with medical problems. For a gambling addict I knew, the most effective therapy was referral to a debt counsellor. For a woman struggling against drug dependency, starving herself to feed her habit, it was referral to a food bank. Having enough food in the cupboard gave her the peace of mind to be able to address her addiction. For a fit, newly retired and newly widowed man I knew, it was volunteering in a charity shop that helped him the most. For someone escaping the stress of an abusive marriage with her three children, it was a phone call to the local branch of Women’s Aid. For an immigrant family living in a damp, cramped slum that was worsening one child’s asthma, it was a letter to the housing department.
Clinicians such as doctors, nurses and physiotherapists drop in and out of patients’ lives so fleetingly that for most people in recovery, the majority of caring work is done by family and friends. Some of my patients over the years have found it difficult to remember the needs and the frustrations of loved ones who are doing the bulk of that work. But the contributions of those around us to healing are irreplaceable, and their resilience is something to be cherished and protected. It, too, may hold the key to recovery.
It is a tyranny to assume that positivity can overcome all obstacles. Much of what constitutes illness consists of things we cannot change. In his book Between Sickness and Health: The Landscape of Illness and Wellness, the rehabilitation specialist Christopher Ward has written of how his first step with a new patient is always to acknowledge their suffering, and to then redefine the goals of treatment not necessarily as “rehabilitation”, but as “possibilitation”: the opportunity of each person to work towards the best possible version of their life.
Even with the advances of 21st-century medical technology, surgery, DNA profiling and gene therapy, the list of illnesses that can be definitively cured is surprisingly short. In terms of drugs or quick fixes, medicine has depressingly little to offer people suffering from long Covid symptoms. But for all that the western medical attitude to the body and illness frequently disappoints, it remains a powerful approach, and for that reason has been adopted in some form or another across much of the globe. Even its ability to define and name our illnesses can offer consolation – I’ve seen many reassured by that act of naming, comforted by the knowledge that what afflicts them has an existence separate from themselves. The naming of an illness offers access to a community of others who have found ways of living with the same difficulties, and that itself can be a source of hope. But there’s a paradox at work: categorising an illness can offer a false sense of definition, locking us into an expectation that becomes self-fulfilling. I’ve known patients who accept the label of an illness with relief, and others who detest all labels as stigmatising. Where possible, I try to take those preferences into account.
The reality of mind and body is one of dynamism and change – any vision of human life that is static at heart is an illusion. Sometimes the most helpful attitude to adopt is not to think of illness categories as concrete, immutable destinies, but as stories of the mind and the body. Within certain impassable limits, stories can be rewritten.
‘Pure, liquid hope’: what the vaccine means to me as a GP Read more
No one is getting any younger, and all of us would do well to remember that health can never be a final destination, but a balance between extremes, different for everyone, and whether we achieve it or not depends on our goals and priorities as much as it depends on anatomy and physiology. Every illness is unique, which means that all recoveries must also be in some sense unique. There is no one-size-fits-all to getting better. And though I have tried to set out some principles that have proven helpful over the years in guiding me, and my patients, through the many landscapes of illness, I’m conscious that it’s possible to touch on only a few waypoints – it’s rarely possible to indicate an easy way out. It’s a landscape we all have to visit sooner or later. From time to time we all need to learn the art of convalescence.
Recovery by Gavin Francis (Profile, £4.99). To support The Guardian and Observer, order your copy at guardianbookshop.com. Delivery charges may apply.
• Follow the Long Read on Twitter at @gdnlongread, listen to our podcasts here and sign up to the long read weekly email here.